Introduction
Multiple myeloma is cancer of plasma cells, a type of white blood cell found mainly in the bone marrow. Normal plasma cells are responsible for producing a mixture of many types of antibodies to protect your body against infections. In multiple myeloma, the abnormal plasma cells multiply uncontrollably and produce large amounts of a single type of antibody called M-protein.
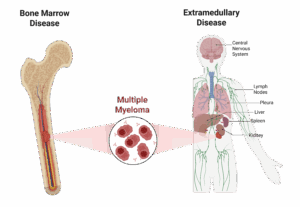
Most of the time, the vast majority of myeloma cells stay inside the bone marrow, but sometimes cancerous plasma cells form masses outside of the bone marrow. When this happens, it is referred to as extramedullary disease (EMD).
What is Extramedullary Disease?
Extramedullary disease (EMD) happens when certain mutations to myeloma cells allow them to leave the bone marrow and spread to other locations in the body (Figure 1). Outside the bone marrow, myeloma cells can form soft tissue tumors without any connection to bone. These tumors spread via the bloodstream to organs like:
- Liver
- Spleen
- Kidneys
- lymph nodes
- Pleura
- Central nervous system (CNS)
EMD can be present at the time of diagnosis, but can also occur at the time of relapse following treatment induced remission. EMD may occur in up to 20% of newly diagnosed multiple myeloma (NDMM) patients and up to 40% of relapsed/refractory multiple myeloma (RRMM).
Figure 1: Illustration of the comparison between bone marrow confined disease and extramedullary disease in multiple myeloma.
Why is Extramedullary Disease a Problem?
EMD is often more aggressive and is consistently associated with an unfavorable prognosis when compared to myeloma cases without EMD , because:
- It’s harder to detect: Diagnosis of EMD can be very difficult due to varying locations and subtle presentation. Standard bone marrow tests can miss it entirely. A patient may have no detectable disease in their marrow, but still have tumors growing elsewhere.
- It can behave differently: Myeloma cells in EMD typically have high risk genetic alterations (RAS/BRAF), increased proliferation, and therapy resistance.
- It raises the risk of relapse: Even if the marrow looks “clean”, EMD is associated with a higher likelihood of quicker relapse and is characterized by a more refractory disease course.
Although novel therapeutic agents are available for EMD patients, it still remains a major clinical challenge, necessitating very close monitoring and individualized treatment plans, depending on disease location, extent, and biology. Localized cases may be treated with radiotherapy (with or without surgery), while systemic involvement requires anti-myeloma chemotherapy, sometimes combined with autologous stem cell transplant (ASCT).
Limitations of Traditional Monitoring for Extramedullary Disease
Doctors rely on minimal residual disease (MRD) testing and imaging scans to track treatment response and look for relapse. While these methods are powerful, some methods don’t catch extramedullary disease (EMD).
Bone marrow-based MRD testing with next-generation sequencing (NGS) or next-generation flow (NGF) is extremely sensitive, capable of detecting even a few cancer cells among thousands to millions of normal marrow cells. But there’s a major limitation: the test only collects cells from a small location within the bone marrow. Since EMD develops outside this space, it can easily be missed. A patient might receive a “negative” MRD result, suggesting remission, even while hidden disease is still active elsewhere in the body.
Imaging adds another layer by looking for tumors in the bones, soft tissues, or organs. Whole body CT scans are quick and widely available, but mainly pick up larger bone damage. PET-CT scans are highly effective for spotting active EMD and provide useful prognostic information, but they involve radiation, are expensive, and not always accessible. Importantly, all these imaging tools can miss very small or low activity lesions, and sometimes they can’t clearly distinguish between active cancer and scar tissue left from earlier treatment.
Catching Extramedullary Disease with Blood-Based MRD Monitoring
Standard blood tests for multiple myeloma, like serum protein electrophoresis (SPEP) or immunofixation, measure the M-protein made by myeloma cells. These tests are useful for diagnosing multiple myeloma and are less invasive than bone marrow biopsies.
But when it comes to monitoring extramedullary disease (EMD), these routine blood tests fall short. They lack the sensitivity to pick up very small amounts of myeloma protein. As a result, EMD may go undetected until it is advanced enough to cause symptoms or show up on imaging.
This is where ultra-sensitive blood-based MRD methods come in, such as clonotypic mass spectrometry (e.g. EasyM). Unlike standard blood tests, EasyM can detect an amino acid sequence “fingerprint” unique to each patient’s M-protein and track it in the blood at incredibly low levels.
Here’s why blood-based MRD monitoring with clonotypic mass spectrometry matters for EMD:
- More sensitive than traditional blood tests or imaging. A positive result of EasyM warrants a more careful search for the evidence of relapse, including the possibility of EMD.
- Whole body coverage since blood flows everywhere, catching signals from marrow and extramedullary sites.
- Less invasive than bone marrow biopsies.
- Individualized for each patient’s unique myeloma clone.
By going beyond the limits of routine blood work, EasyM could provide an early warning system for EMD, helping doctors catch hidden disease before it becomes symptomatic or harder to treat.
Key Takeaways
Current monitoring with bone marrow tests does not work for extramedullary disease (EMD), which often remains hidden until symptoms develop. Ultra-sensitive blood-based MRD tools, such as clonotypic mass spectrometry (EasyM), can detect very low levels of M-protein, cover the whole body, and reduce reliance on invasive biopsies.
Disclaimer
This article is intended solely for educational and informational purposes. It is not a substitute for professional medical advice, diagnosis, or treatment recommendations. Always seek the guidance of a qualified healthcare provider with any questions you may have regarding a medical condition. Do not ignore or delay seeking medical advice based on content presented here.